Our latest Quick Poll results Participants shows Network dentists are driven by their dedication to improving patient care and keeping up with the latest clinical advancements. However, they face challenges such as time constraints and difficulties with patient recruitment.
Quick Poll Results: Practitioners’ Mixed Responses to New Radiographic Safety Guidelines

Authors: Dr. Joana Cunha-Cruz & Brittni Ball
Introduction
The American Dental Association (ADA) has updated its guidelines on dental radiographic examination. We conducted a Quick Poll with members of the National Dental PBRN to assess the practices of dental practitioners related to radiographic safety and their knowledge about the updated ADA guideline.
Methods
Study Design and Participants: This was a cross-sectional survey providing preliminary data for future studies. Dental practitioner members of the National Dental Practice-Based Research Network in the United States were invited to complete the Quick Poll.
Data Collection: Members of the network were invited to complete an online survey through email. Two email invitations were sent to all members: one in the network’s monthly newsletter sent on May 2, 2024, and one as a follow-up email sent on May 10, 2024. The Quick Poll was open from May 2 through May 18, 2024. The page was opened 1,527 times and the survey was completed 312 times.
Measures and Data Analysis: The survey asked dental practitioners about their practices in radiographic safety and their knowledge about the guideline. Questions included awareness of the guideline, agreement with recommendations, and usage of radiographic techniques and safety practices. The data were collected through a web survey in Constant Contact, a digital and email marketing platform. Data were analyzed using descriptive statistics.
Results
Highlights
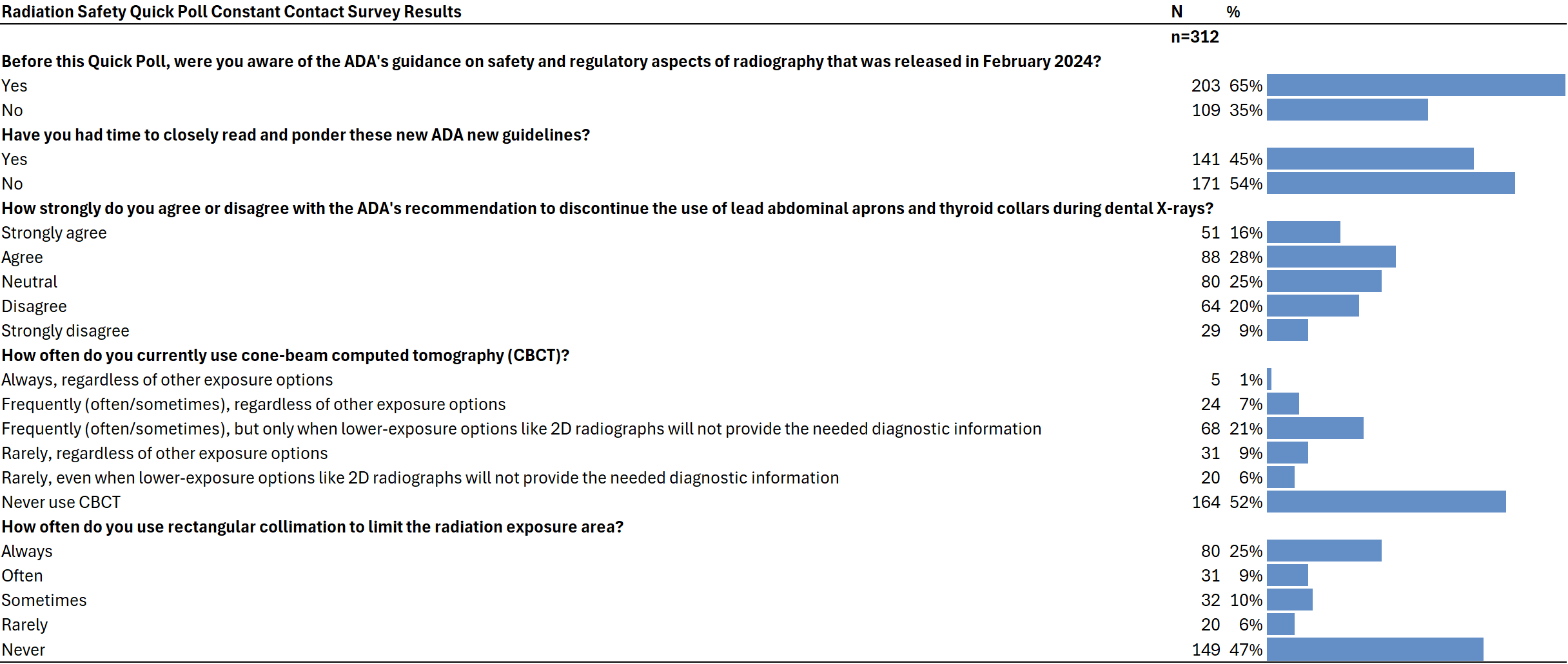
- 65% of respondents were aware of the guidelines
- While 44% agreed or strongly agreed with the recommendation to discontinue the use of lead abdominal aprons and thyroid collars during dental X-rays, 25% were neutral and 29% disagreed or strongly disagreed with these recommendations
Of the 312 respondents, 65% were aware of the ADA’s updated guidance on safety and regulatory aspects of radiography, while 35% were not aware. Less than half of the practitioners who answered the QP had closely read the guidelines.
In relation to the discontinuation of the use of lead abdominal aprons and thyroid collars during dental X-rays, 44% agreed or strongly agreed with these ADA’s recommendations, 25% were neutral, and 29% disagreed or strongly disagreed with these recommendations.
Almost half of the practitioners (52%) never use cone-beam computed tomography (CBCT). One-fifth (21%) used CBCT more frequently, but only when lower-exposure options like 2D radiographs will not provide the needed diagnostic information. Fifteen percent rarely used CBCT, and 8% frequently or always used CBCT, regardless of other exposure options.
About one-third of the practitioners reported using rectangular collimation (25% always, 9% often). Most practitioners reported using it less frequently, with 16% using it sometimes or rarely, and 47% never using rectangular collimation.
Table 1
Conclusions
The survey results provide valuable insights into how dental professionals align with the updated ADA guidelines on radiographic safety and regulatory practices. A significant majority (65%) of respondents were aware of the ADA’s updated recommendations, though less than half had closely reviewed them. This suggests that while awareness is relatively high, deeper engagement with the guidelines can be improved.
The ADA emphasizes a patient-centered approach, advising against the routine use of lead abdominal aprons and thyroid collars due to advancements in digital X-ray technology and beam restriction. The survey findings reflect some alignment with this guidance, as 44% of practitioners agreed or strongly agreed with discontinuing these protective measures, although a notable 29% disagreed, indicating room for further education and consensus-building.
The use of Cone-Beam Computed Tomography (CBCT) also demonstrates partial adherence to the ADA’s recommendations. The guidelines advocate for CBCT only when lower-exposure options like 2D radiographs are insufficient. The survey revealed that 52% of practitioners never use CBCT, while 21% use it selectively under these conditions, aligning well with the ADA’s emphasis on minimizing radiation exposure. However, 8% of practitioners reported frequent or consistent use of CBCT regardless of other options, which may indicate a need for further emphasis on judicious use to comply with safety recommendations.
Rectangular collimation, another key aspect of the ADA guidelines aimed at reducing radiation exposure during intraoral imaging, appears underutilized among practitioners. Only 34% reported using it always or often, while nearly half (47%) never use it. While the low adoption of rectangular collimation underscores the need for enhanced training and awareness, practical challenges may also play a role in limiting its implementation. Factors such as equipment compatibility and accessibility of collimators for certain types of X-ray systems could contribute to the reported underutilization. For instance, some practitioners may encounter difficulties sourcing collimators for wall-mounted units, which could impede their ability to follow the guidelines fully.
Addressing these barriers will require a multifaceted approach that not only emphasizes the importance of radiation safety but also considers the logistical and technological constraints faced by dental practices. Ultimately, these findings highlight an opportunity for further dialogue between practitioners, manufacturers, and professional organizations to identify solutions that facilitate compliance with updated guidelines. Through such collaboration, the dental community can advance both safety standards and practical implementation, ensuring optimal outcomes for patients and providers alike.
Read the ADA publication to learn more
Benavides E, Krecioch JR, Connolly RT, Allareddy T, Buchanan A, Spelic D, O’Brien KK, Keels MA, Mascarenhas AK, Duong ML, Aerne-Bowe MJ, Ziegler KM, Lipman RD. Optimizing radiation safety in dentistry: Clinical recommendations and regulatory considerations. J Am Dent Assoc. 2024 Apr;155(4):280-293.e4. doi: 10.1016/j.adaj.2023.12.002. Epub 2024 Feb 1. Erratum in: J Am Dent Assoc. 2024 Jun;155(6):A8. doi: 10.1016/j.adaj.2024.04.003. PMID: 38300176.
Additional Resources from ADA
See past Quick Polls
Click here to view a list of all of our past Quick Polls and their results.
Interested in Becoming a Member?