We are thrilled to share some significant leadership updates within our network. These changes mark a new chapter of growth and excellence, and we are excited to introduce the individuals stepping into their new roles.
Beyond the Chair: Dentists’ role in mental health and smoking cessation

Authors: Dr. Sandra Japuntich and Carina Lundtvedt, MSW
Dentists have a significant role in not just oral health, but overall patient health. This includes screening for mental health issues and smoking habits. By identifying these risks and referring patients to community resources, dentists can help mitigate the high smoking rates among individuals with mental illnesses. Offering smoking cessation options further enhances their role in improving both physical and mental health outcomes. This approach ensures health equity, providing equal care for all, including those with mental illnesses.
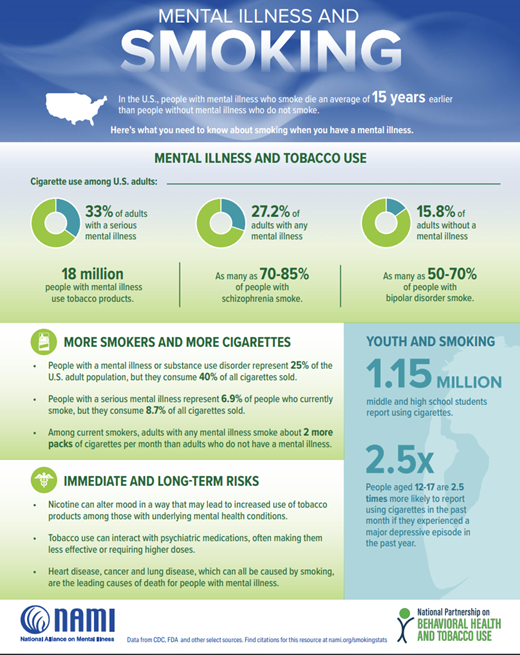
Cigarette smoking is a known risk factor when it comes to both physical and mental health. Smoking rates are disproportionally higher in those living with a mental illness (depression, anxiety, PTSD, schizophrenia, etc.) than those who do not. People living with mental illness are four times more likely to die prematurely from smoking related diseases (NAMI, 2021). See infographics courtesy of the National Alliance on Mental Illness (2021). Individuals living with a mental illness may use smoking cigarettes as a way to self-medicate. However, cigarette use can make mental health symptoms worse. Similarly, there is no evidence that quitting smoking is associated with deteriorations in mental health and some evidence that mental health symptoms improve after cessation.
People with mental illness are as motivated to quit as those without. Smoking cessation treatments including medication and counseling are as effective in people with vs. without mental illness. Some state quitlines offer mental health tailored counseling programs. While providers sometimes are concerned about addressing smoking with their patients with mental illness out of concerns that that smoking is the least of their problems, it is a critically important equity issue that people with mental illness get the same care for smoking as anyone else.
Quick tips for addressing smoking in people with a history of mental illness:
- Do not assume your patient is not interested in quitting smoking.
- Smoking cessation counseling and medication work for people with mental illness. Follow the same Ask-Advise-Refer protocol.
- State quitlines may offer expanded services for people with mental illness. Encourage patients to be honest about their mental health history with quitline staff to access these programs.
- People with mental illness may prefer to gradually reduce rather than abruptly quit smoking. Ask patients if they want to make changes to their smoking rather than if they want to quit smoking.
- Approach all conversations about tobacco use with empathy and understanding.
Resources
Behavioral Health & Tobacco Use. (n.d.). Www.lung.org. https://www.lung.org/quit-smoking/smoking-facts/impact-of-tobacco-use/behavioral-health-tobacco-use
Smoking | NAMI: National Alliance on Mental Illness. (2021). Nami.org. https://www.nami.org/About-Mental-Illness/Common-with-Mental-Illness/Smoking
Interested in Becoming a Member?